
Ensuring the Right to Quality Hormonal Implant Removal Services
Over the last decade, the use of contraceptive hormonal implants has risen worldwide,
especially in Sub-Saharan Africa and Asia. These implants are easy-to-use and reliable,
providing women and couples another option for effective, reversible contraception. By
2015, more than 10.5 million implants were distributed in resource-constrained environment
s throughout Africa and Asia, a 130% increase from three years prior in 2012.
With an increase in the use of hormonal contraceptive implants, the need to ensure
access to quality implant removal services (an integral aspect of quality services) is
evident. To expand these services, EngenderHealth is working with the Global Implant
Removals Task Force to identify best practices for implant removals, including those
related to capacity building, service provision, and research and data collection.

Notably, EngenderHealth’s Expand Family Planning project (ExpandFP) has systematically implemented interventions to expand implant insertion and removal services (as well as other family planning services) in the Democratic Republic of the Congo, Tanzania, and Uganda. The project utilizes EngenderHealth’s Supply–Enabling Environment–Demand (SEED)Programming Model, engaging a holistic approach to ensure that proper supply, enabling environment, and demand components are in place to ensure access to implant insertions, removals, and other family planning services. Between January 2014 and June 2016, ExpandFP worked to engage communities, improve service capacity through training and supervision, and increase service delivery to help more than 135,000 women obtain hormonal implants. ExpandFP also facilitated access to removal services for over 4,000 women. In a three country study on client perceptions of quality and choice, a large majority of implant adopters interviewed said they were given essential information on the benefits of implants, on when and where to get the implant removed, and on their right to removal at any time.
EngenderHealth has released Contraceptive Hormonal Implant Removal Services: Experiences
from the ExpandFP Project in the Democratic Republic of the Congo, Tanzania, and Uganda, a brief developed to assist those engaged in family planning policy and program planning, implementation, and management to understand what needs to be in place to ensure access to removal services. The brief also expands on recent increases in implant use, as well as on the ExpandFP experience described above.
It Takes a Village: Results from the Expand Family Planning Project in Tanzania
Like so many around the globe, I have spent recent weeks cheering on athletes at the 2016 Olympics in Rio de Janeiro. These athletes are real-life superheroes. Take Simone Biles, who has won the most Olympic and world championship medals ever won by an American gymnast—simply amazing. Watching the Olympics, I am inspired by and in awe of the dedication and effort needed to succeed—not just by the athlete but also all the people who helped make that success happen, including family, coaches, doctors and therapists, fans, and so many more. It is that same collective commitment by many working toward a shared goal that achieves results, no matter what the industry or field.
It is in this spirit of collective effort by a village of actors that I am very pleased to share key results from the Expand Family Planning (ExpandFP) project in Tanzania. Led by EngenderHealth, the ExpandFP project ensures clients’ full, free, and informed choice of contraceptive method while expanding the availability and use of long-acting reversible contraceptives (LARCs)—i.e., hormonal implants and intrauterine devices (IUDs). Funded by the Bill & Melinda Gates Foundation, ExpandFP is part of the global FP2020 effort to provide contraception to an additional 120 million women and girls in the world’s poorest countries by 2020. The project focused on:
- Training health care providers and managers in family planning (FP)
- Improving service quality and supervision
- Ensuring clients’ rights and choice, medical follow-up care, and access to implant and IUD removal services on demand
- Using data for decision-making, particularly for contraceptive security
- Reaching communities with FP information; supporting community health workers and volunteers; and engaging community leaders to support FP efforts
Translating Global Family Planning Commitments into Local Action: The ExpandFP Project in Uganda, Tanzania, and the DRC
When I think about how far the global family planning (FP) community has come since the first International Conference on Family Planning (ICFP) in 2009, I am amazed by the progress to date. Like many of my colleagues in the field, we have seen significant momentum since FP2020 and increased resources toward improving women’s access to FP.
Equally critical to achieving the FP2020 goal of reaching 120 million new FP users, however, is how efforts are undertaken. That is why EngenderHealth, along with its partners, has taken deliberate steps toward ensuring that FP services are designed, implemented, and monitored in a way that protects women’s rights and puts their needs, desires, and preferences at the center.
(more…)
Checkpoints for Choice: A New Orientation and Resource Package for Ensuring Voluntary Family Planning Programs
How can stakeholders ensure that family planning programs are designed, implemented, and monitored in a way that respects, protects, and fulfills human rights and puts clients’ needs and preferences at the forefront?
 With a renewed global commitment to family planning (FP) among donors and governments worldwide, momentum is growing to support practical ways to infuse a human rights approach into voluntary FP programs. In support of these efforts, EngenderHealth recently published Checkpoints for Choice: An Orientation and Resource Package, a new publication (also available in French) that offers practical guidance on how program planners and managers, policymakers, donors, service providers, community leaders, to strengthen clients’ ability to make full, free, and informed contraceptive choices within a rights-based context.
With a renewed global commitment to family planning (FP) among donors and governments worldwide, momentum is growing to support practical ways to infuse a human rights approach into voluntary FP programs. In support of these efforts, EngenderHealth recently published Checkpoints for Choice: An Orientation and Resource Package, a new publication (also available in French) that offers practical guidance on how program planners and managers, policymakers, donors, service providers, community leaders, to strengthen clients’ ability to make full, free, and informed contraceptive choices within a rights-based context.
Behavioral change communication is critical for the success of voluntary and choice-based family planning programs
Guest post by Banchiamlack Dessalegn, Ph.D., Senior Technical Advisor for Monitoring, Evaluation and Research, Family Health International 360 (FHI 360), Addis Ababa Ethiopia
Knowledge and awareness of available family planning (FP) methods, as well as of their benefits and side effects, is a prerequisite for informed decision making (Bongaarts et al., 2012). Behavior change communication (BCC) is a tool for increasing knowledge and awareness. In this way, BCC can be seen as critical to facilitating successful voluntary, choice-based FP.
The Government of Ethiopia aims to increase the modern contraceptive prevalence rate (mCPR) to 55% by 2020, as stated in Ethiopia’s new Health Sector Transformation Plan. To achieve this, the Federal Ministry of Health (FMOH) is putting emphasis on improving the FP method mix, including by increasing demand for and access to long-acting and permanent methods of FP (LA/PMs) without compromising informed and free choice. While target-setting at the national and subnational levels might lead to the erosion of choice-based FP services, the FMOH has given clear direction that services must be based on proper counseling and free choice. As a result of the concerted efforts and results-oriented policies of the FMOH, impressive achievements have been made in recent years, with the mCPR increasing from 28.6% in 2011 to 41.8% in 2014 and the total fertility rate dropping from 4.8 to 4.1 lifetime births per woman during the same period (CSA [Ethiopia] & ICF International, 2012; CSA [Ethiopia], 2014).
A means to an end, or an end in itself? Rights, access, and comprehensive sexuality education
Guest post by Heather Barclay, International Planned Parenthood Federation
Comprehensive sexuality education (CSE) has been the focus of much discussion and political debate over the years. It has been lauded as the way for young people to be empowered and realize their rights, as well as a means through which to create demand for family planning and sexual health services. But as with many highly politicized debates, the truth lies somewhere in the middle.
A hallmark of CSE is its rights-based approach to education about sexuality, gender, sexual and reproductive health, and sexual behavior. It equips young people with life skills and empowers them to make autonomous, informed decisions about their bodies and futures. That means teaching young people comprehensively both about the biology of sex and about the personal, emotional, societal, and cultural forces that shape the way in which they choose to conduct their lives, including their sexual and reproductive lives. In particular, CSE imparts information, promotes responsibility, and equips youth to question why they act in certain ways, so that they can make informed and considered decisions that allow them to have healthy and empowered lives.
Marie Stopes International and EngenderHealth lead endeavor to expand contraceptive choice
by Sara Malakoff, Senior Program Associate, EngenderHealth
Female sterilization is the world’s most popular contraceptive method with more than 220 million users. Sterilization is convenient for women who desire to limit childbearing, as it requires no further visits to a health care provider. In addition, it does not have the side effects that contribute to the discontinuation of user dependent methods, such as hormonal contraception. However, access to both male and female sterilization varies significantly geographically, is limited in many parts of the world (particularly in rural areas), and has not increased at a pace comparable to that of the unmet need to limit childbearing.
In an attempt to address issues of full contraceptive choice and to ensure the availability of and access to a wide range of contraceptives, including permanent methods, Marie Stopes International (MSI) and EngenderHealth under the auspices of the Support for International Family Planning Organizations (SIFPO) project funded by USAID, convened a two-day technical symposium in Nairobi in March 2014 entitled Provision of Permanent Methods of Contraception in Low-Resource Settings. A dynamic group of over 40 participants from 27 organizations and 13 countries attended the event.
Gender Norms and Power Inequities: Key Barriers to Realizing Sexual and Reproductive Rights

Guest post by Christina Wegs, Senior Advisor for Global Policy and Advocacy, CARE
December 10th was International Human Rights Day. This day commemorates the adoption of the Universal Declaration of Human Rights (UDHR) by the UN General Assembly in 1948, which affirmed the rights of all people, everywhere and all the time. The Declaration, as well as similar international treaties and agreements, confirm the centrality and importance of protecting and fulfilling sexual and reproductive rights (SRR). Embraced within the concept of SRR is the right to reproductive self-determination; the right to sexual and reproductive health (SRH) information, education, and services; the right to the highest attainable standard of health; and the right to equality and non-discrimination.
Despite international recognition of the importance of SRR, sixty years on and twenty years after the International Conference on Population and Development, women and girls in every part of the world continue to face considerable barriers to realizing their SRR. In many places, unmarried women and adolescents are denied access to reproductive health information and services, many women are not able to exercise full, free, and informed contraceptive choice, and women continue to die from preventable complications of pregnancy and childbirth. Pervasive gender inequality limits women’s decision-making autonomy and undermines their health and well-being throughout their lives. Finally, many women—especially poor and socially marginalized women—continue to experience systemic discrimination in health care, which not only results in poor quality of care and poor health outcomes, but also acts as a powerful disincentive to women seeking care.
When Everything Must Go Right So Nothing Goes Wrong
By Pamela Barnes, President & CEO, EngenderHealth
In global health, nobody has an easy job, but ensuring voluntary and safe permanent contraception is among the toughest. Everything has to go right so that nothing goes wrong.
The latest disturbing news coming from Chhattisgarh, India, reminds us that despite being 20 years post-ICPD, we global health professionals have more to do to ensure reproductive rights, choice, and quality of care. And as the story goes—as it has too many times before—the devastating consequences are borne by mostly poor, rural women. It’s unconscionable.
Although the Chhattisgarh situation is under investigation by the Government of India, we know that quality of care was compromised at all levels. This includes the conditions under which the surgical sterilizations were performed, the high number of surgeries in a given period, the questionable quality of the medications, the implicit targets set by local authorities, and financial incentives. In many ways, there isn’t a simple answer to what happened–there were a series of systemic, programmatic and clinical failures. Many organizations, including EngenderHealth, have called for a greater need to ensure and protect human rights, reproductive rights and clients’ rights; and to address informed and voluntary decision making, counseling, client safety and service quality.
But how does this translate into action? What must go right so that nothing goes wrong?
EngenderHealth’s commitment to getting everything right, beginning with our work in voluntary permanent methods decades ago, has led to the development of standards used throughout the field for informed consent, clinical safety, infection prevention, and other aspects of quality service delivery. These have also been applied to broader family planning and reproductive health issues. What we’ve learned is that investments must take place at all levels – beginning with a fundamental recognition that individuals have a basic right to full and appropriate information about their reproductive health choices and that they are able to make decisions without coercion, pressure, or inducements. For EngenderHealth, it’s about achieving a vision of client-centered care and all that is meant by this term.
For example, in India it would mean expanding the contraceptive method mix in the public sector, ensuring quality, and working to advocate for a focus to be on client’s choices rather than achieving targets. Right now, it’s mostly sterilization services, intrauterine devices (IUDs), condoms and pills—a situation which limits choice for women and others, including unmarried adolescents. We also see a greater need for training so that service providers are equipped with skills to provide voluntary, safe and quality services and can monitor quality, rights and choice for continuous quality improvement. These are examples of the kinds of concrete actions that must be undertaken as part of a broader comprehensive strategy rooted in a rights-based approach.
The incident in Chhattisgarh is a sobering reminder of what can happen when family planning services are not designed, implemented, or monitored in a way that protects and fulfills individual’s human rights. We urge the Ministry of Health and state governments to take decisive action to develop practical approaches for infusing a rights-based approach, with quality of care as one of the top priorities and with women’s needs, desires, and preferences at the center. To do otherwise would simply maintain the status quo.
—–
EngenderHealth and its partners have developed two new publications to assist diverse audiences, including donors, policymakers, program planners and managers, service providers, rights advocates, and community members, in their efforts to achieve rights-based family planning programs.
The first publication is the Voluntary Rights-based Family Planning Conceptual Framework User’s Guide, a practical resource to help stakeholders design, implement, and monitor family planning programs that respect, protect, and fulfill human rights. Coauthored with the Futures Group, with support from the Bill & Melinda Gates Foundation, the guide is a companion to the recent publication of Voluntary Family Planning Programs that Respect, Protect, and Fulfill Human Rights: A Conceptual Framework, which took long-standing family planning concepts, such as quality of care, voluntarism, and service access and linked them with human rights principles, such as empowerment, equity, nondiscrimination, and accountability. The Framework provides a holistic vision of what a rights-based family planning program looks like; the User’s Guide provides a pathway to applying the framework in actual practice.
EngenderHealth also developed Checkpoints for Choice: An Orientation and Resource Package, which takes a closer look at the concept of voluntarism—one component of a rights-based approach—and helps stakeholders understand the clients’ experience and their ability to make full, free, and informed choices about family planning. The tool, developed with support from the William and Flora Hewlett Foundation and the United States Agency for International Development, consists of a detailed plan with all support materials for a one-day workshop to enable family planning program planners and managers to strengthen the focus of family planning programs on clients’ ability to make full, free, and informed contraceptive choices in the context of a rights-based program. In addition to the workshop guidance and materials, the package includes links to recommended references, tools, and additional reading.
Health in hand: New contraceptive option expands access to family planning
Guest post by Sara Tifft, Project Director, PATH Sayana® Press Pilot Introduction project
Worldwide, women choose injectable contraceptives because they are safe, reliable, and discreet. In many rural or remote areas, however, travelling to a clinic to receive an injection is costly and burdensome. PATH, an international nonprofit health organization, is collaborating with global partners to address this challenge. We began with a basic question: What would it take to deliver more injectable options to women, particularly outside the clinic setting?
One answer is Sayana® Press: a small, easy-to-use injectable contraceptive that has the potential to increase access and choice for millions of women worldwide.

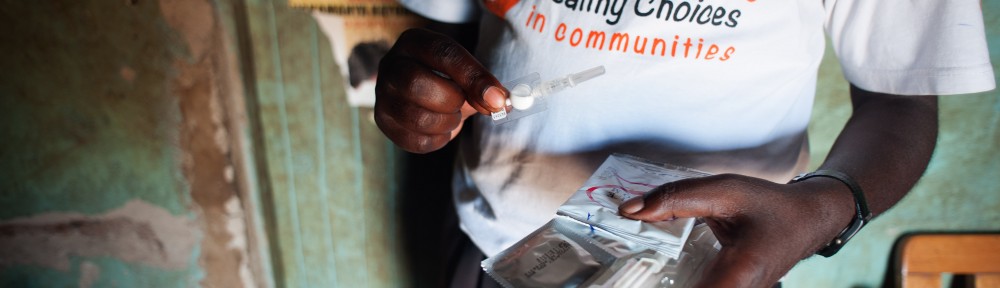
PATH is training community health workers in the Mubende district of Uganda to expand access to family planning, including the Sayana Press injectable contraceptive shown here. Photo credit: PATH/Will Boase


